Vaccines are intended to prepare your immune system to fight off infections and prevent disease. But do you know how they do it exactly?
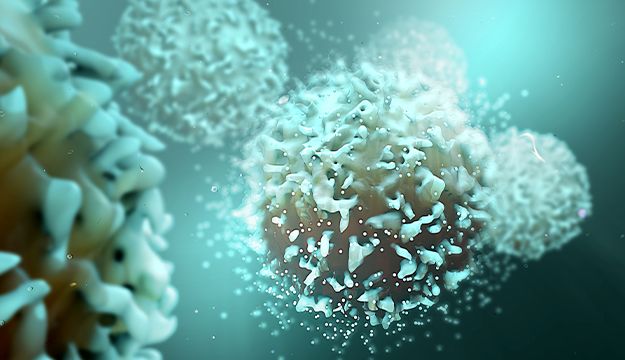
The Human Immune System and Infectious Disease
The human immune system is essential for our survival in a world full of potentially dangerous microbes.
Passive Immunization
You don't always need to be exposed to a pathogen, or part of it, to be immune. Sometimes, an infusion of antibodies from a donor is enough to give you immunity.
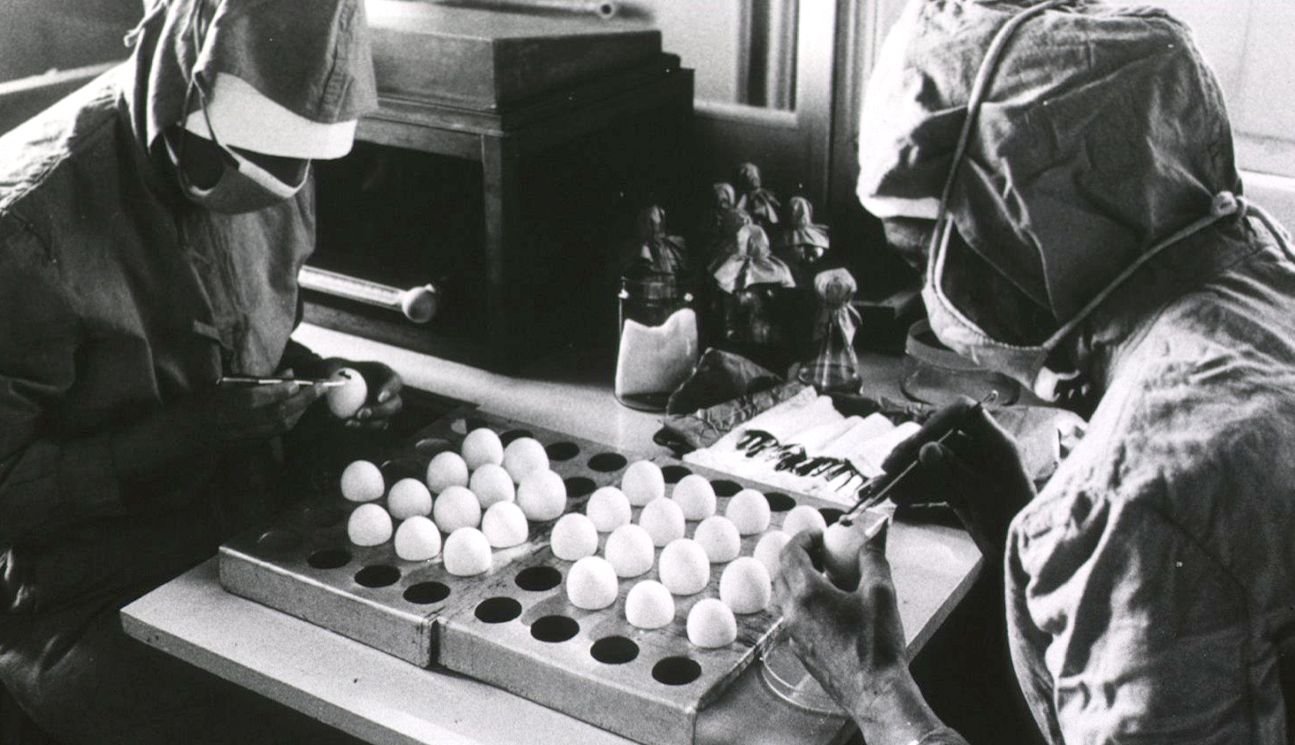
Different Types of Vaccines
There are several types of vaccines, each created in a different way and for a different purpose.
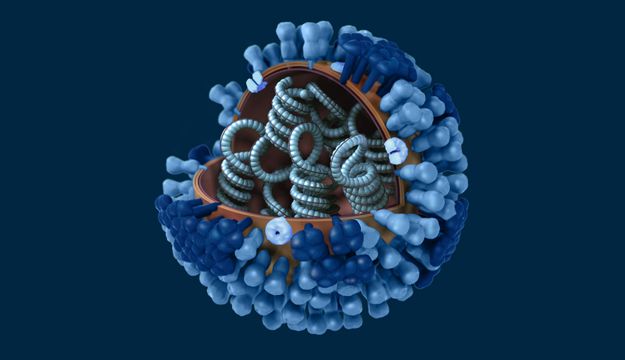
Viruses and Evolution
Pathogens are always evolving, adapting to the pressures put on them by their environment. This could be a problem.

Disease Elimination and Eradication
Eradication means the disease is no longer found anywhere in the world. Only two diseases have been eradicated: one human and one in animals.